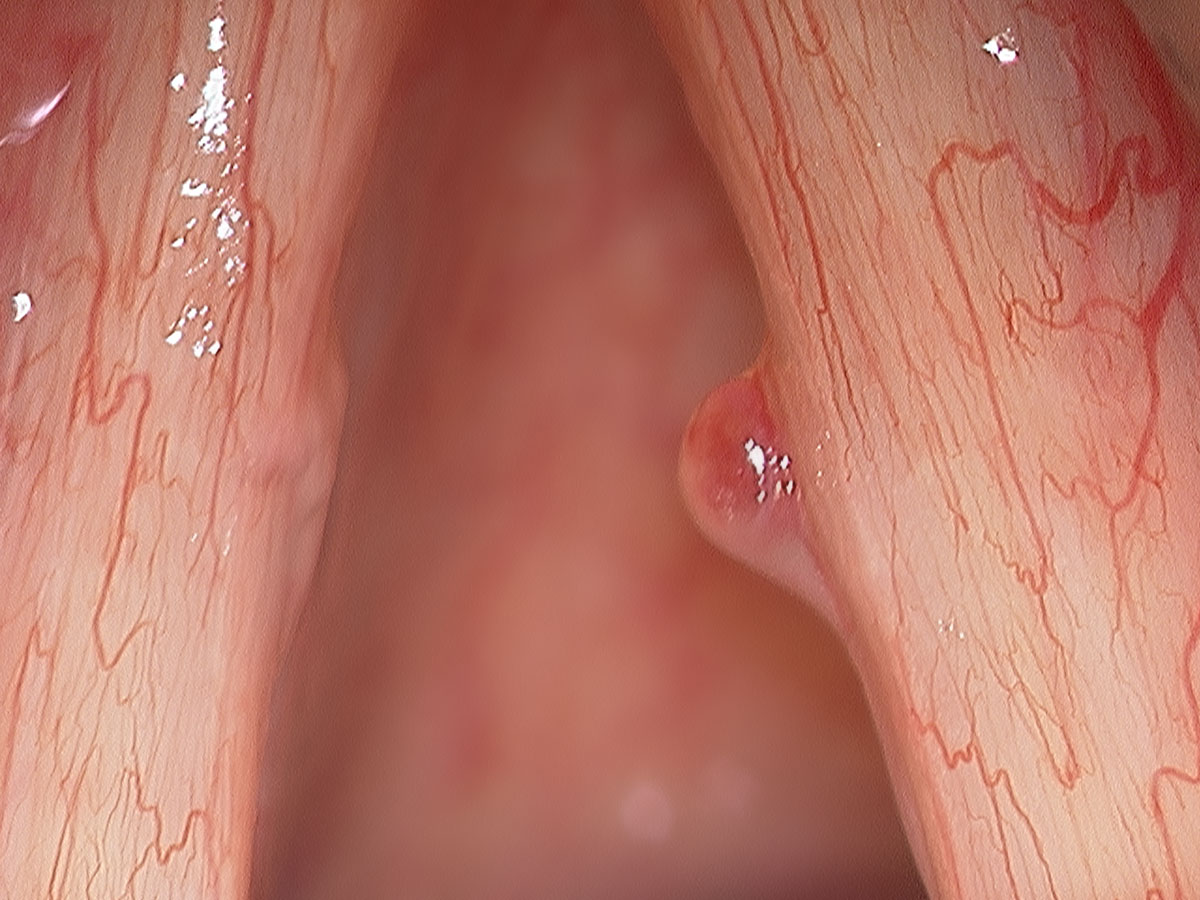
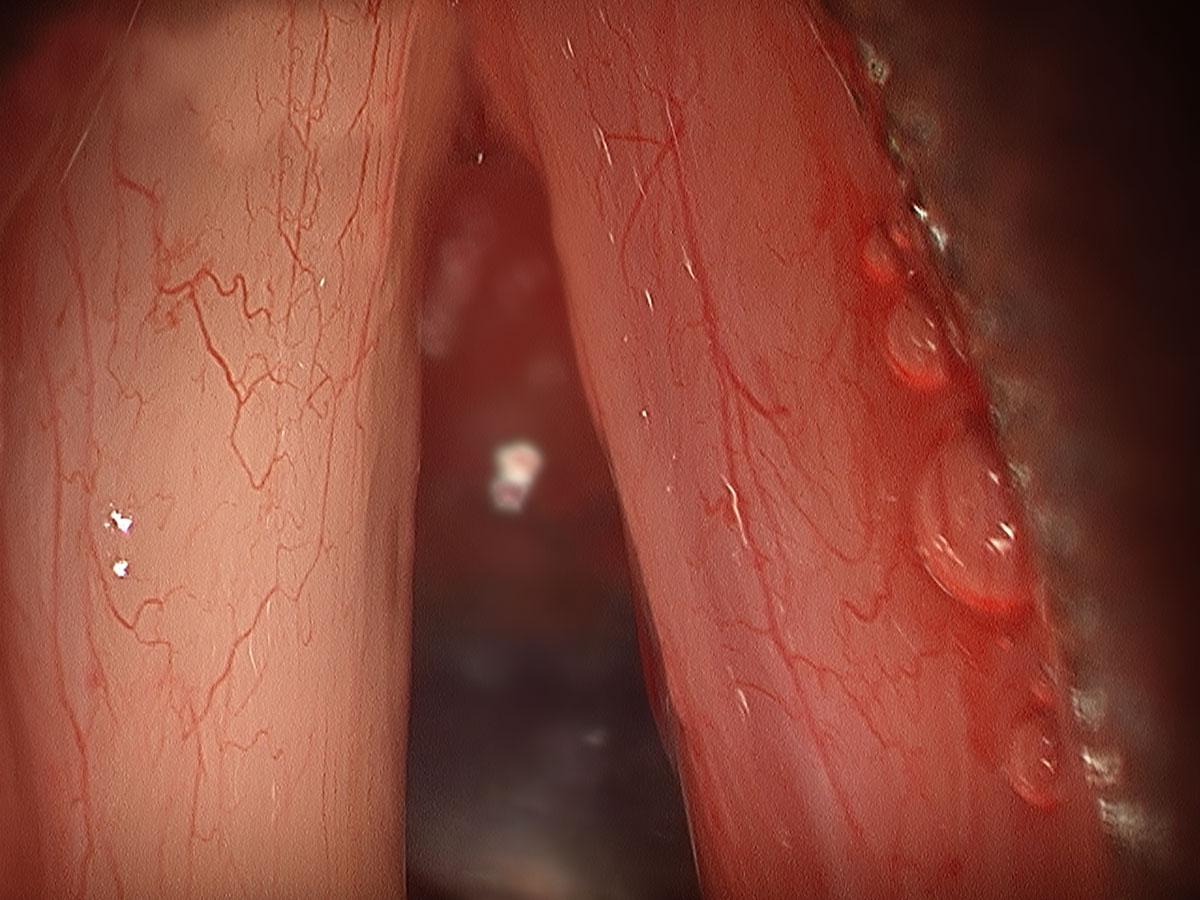
These lesions are considered phonotraumatic lesions. As such, they develop in the setting of repeated vocal fold trauma. This can be over a very brief episode involving substantial coughing with a cold over a week. They can also form from more prolonged voice over-use over many months. Either way, the lesion creates incomplete closure of the vocal cords and alters the surface pliability. As such, it then generates hoarseness by making the vocal cord closure an incompetent valve.
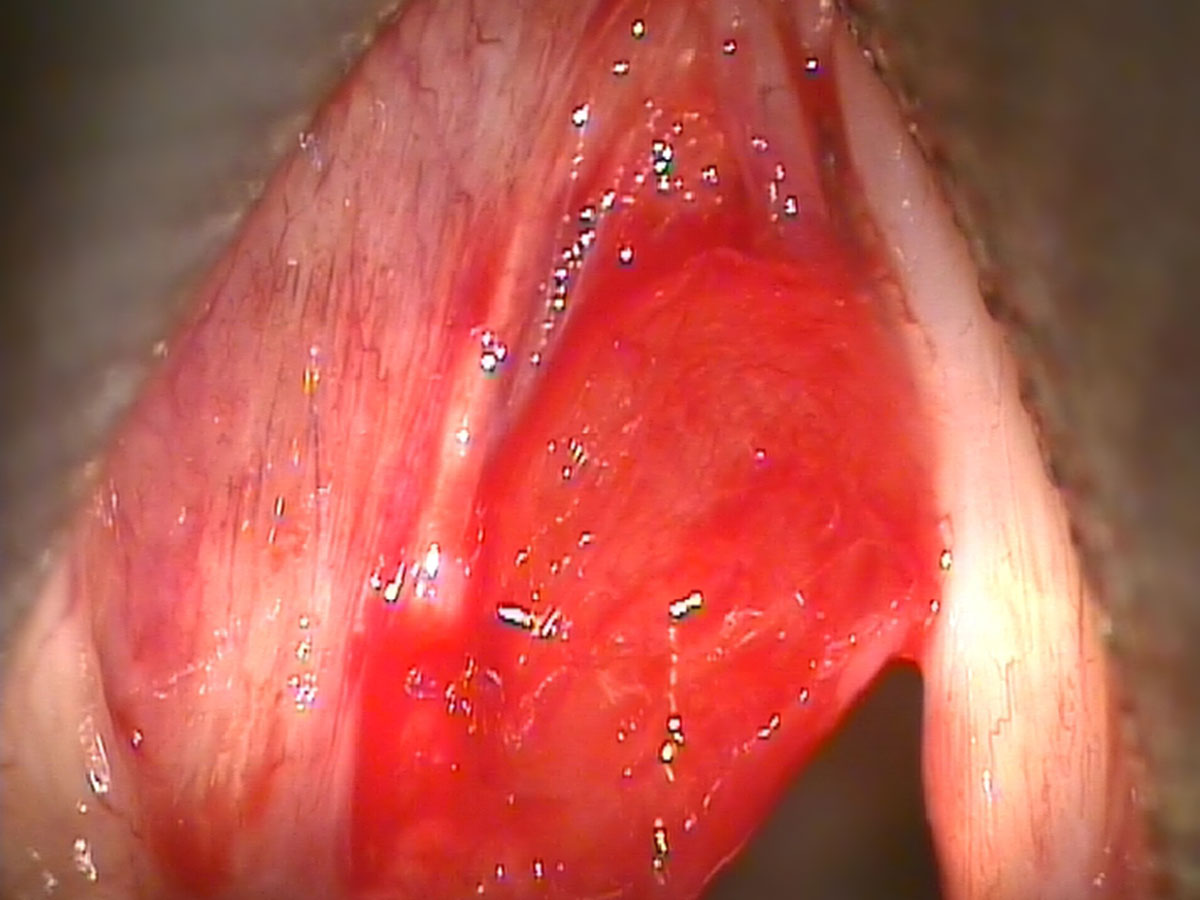
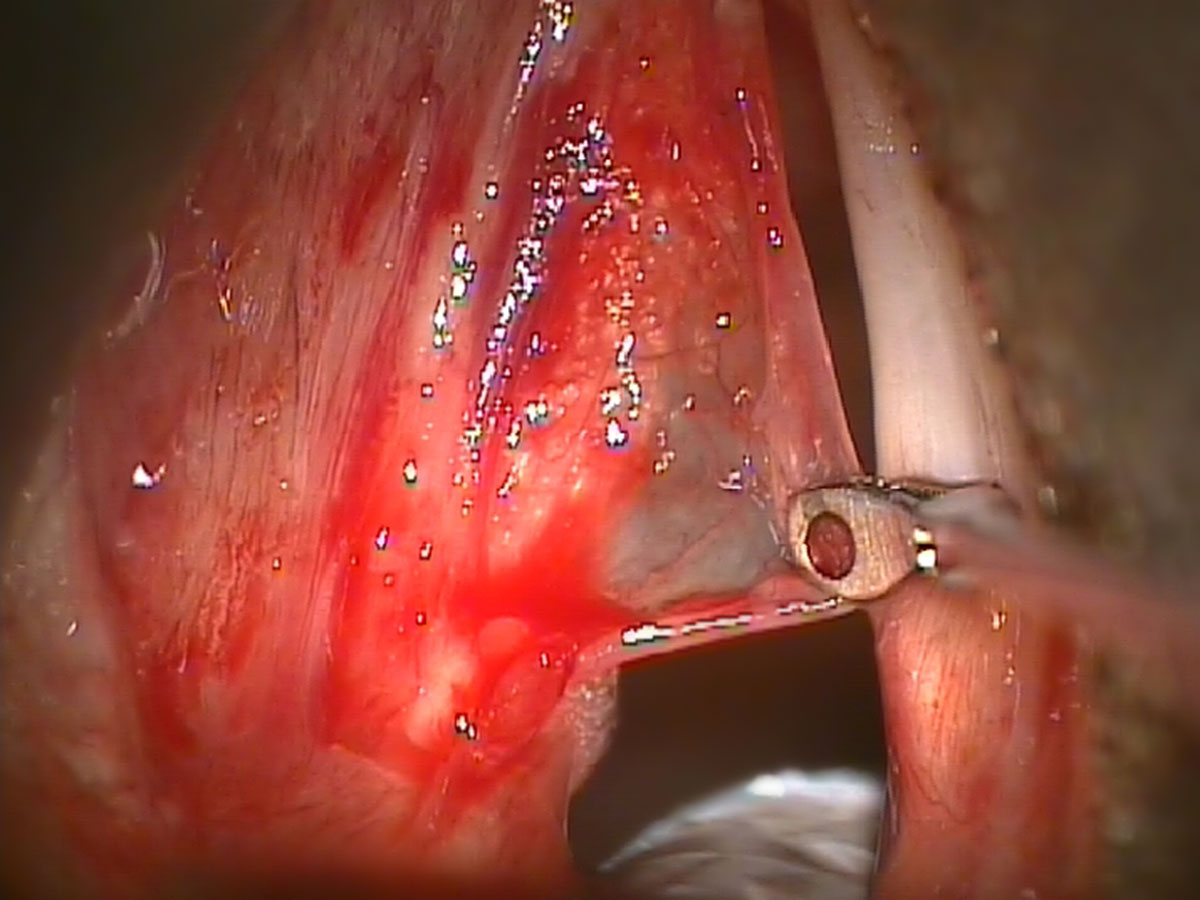
It is critical in the assessment of the hoarse patient to perform a close proximity, high magnification and high definition videostroboscopy. This provides microscopic detail of the lesion and the status of the surrounding tissue of the vocal cords. As such, specific speech therapy or surgery can be safely planned.
All patients require a complete assessment by a highly qualified speech therapist prior to any surgery. It is Dr Broadhurst’s philosophy that single sided vocal fold lesions are best managed with surgery initially followed by intensive speech therapy. This is also the view held by the majority of well-established and respected laryngeal surgeons.
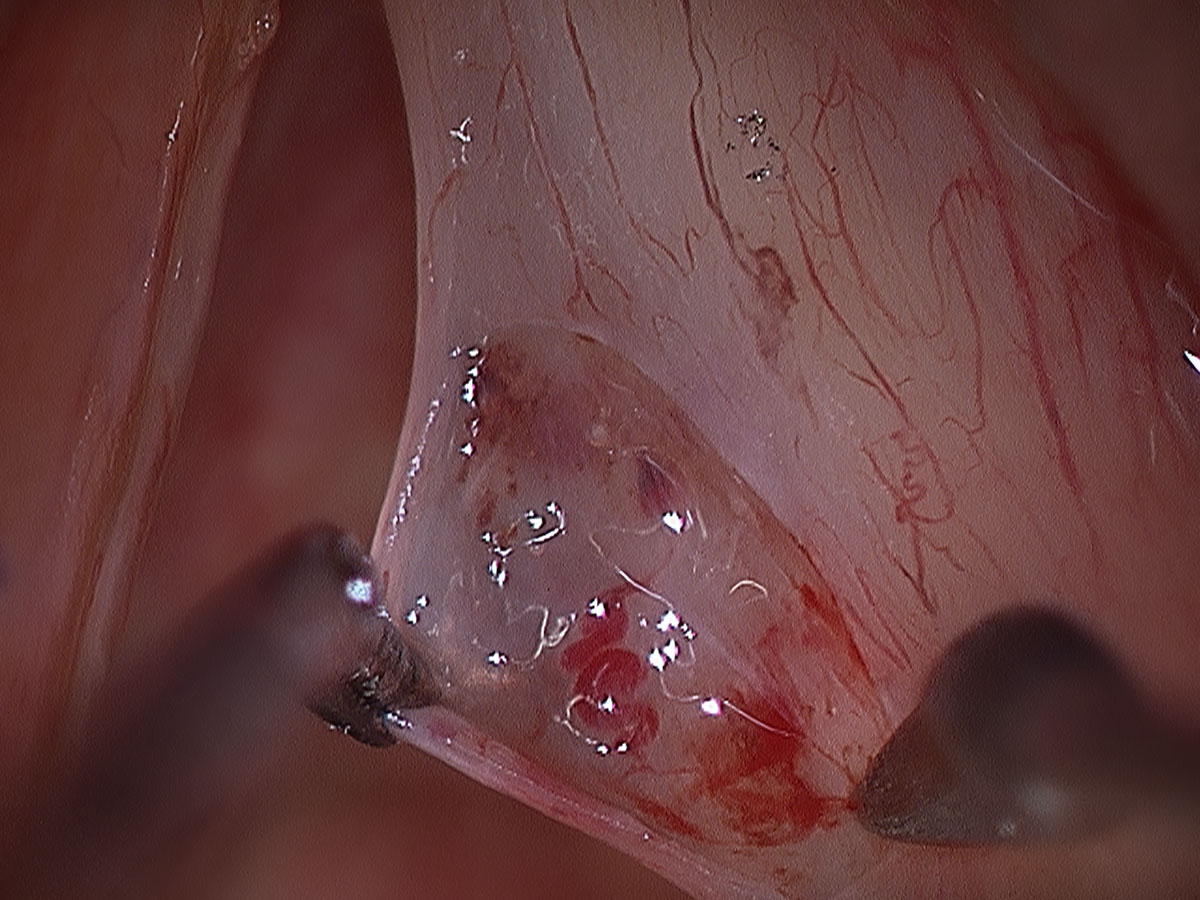
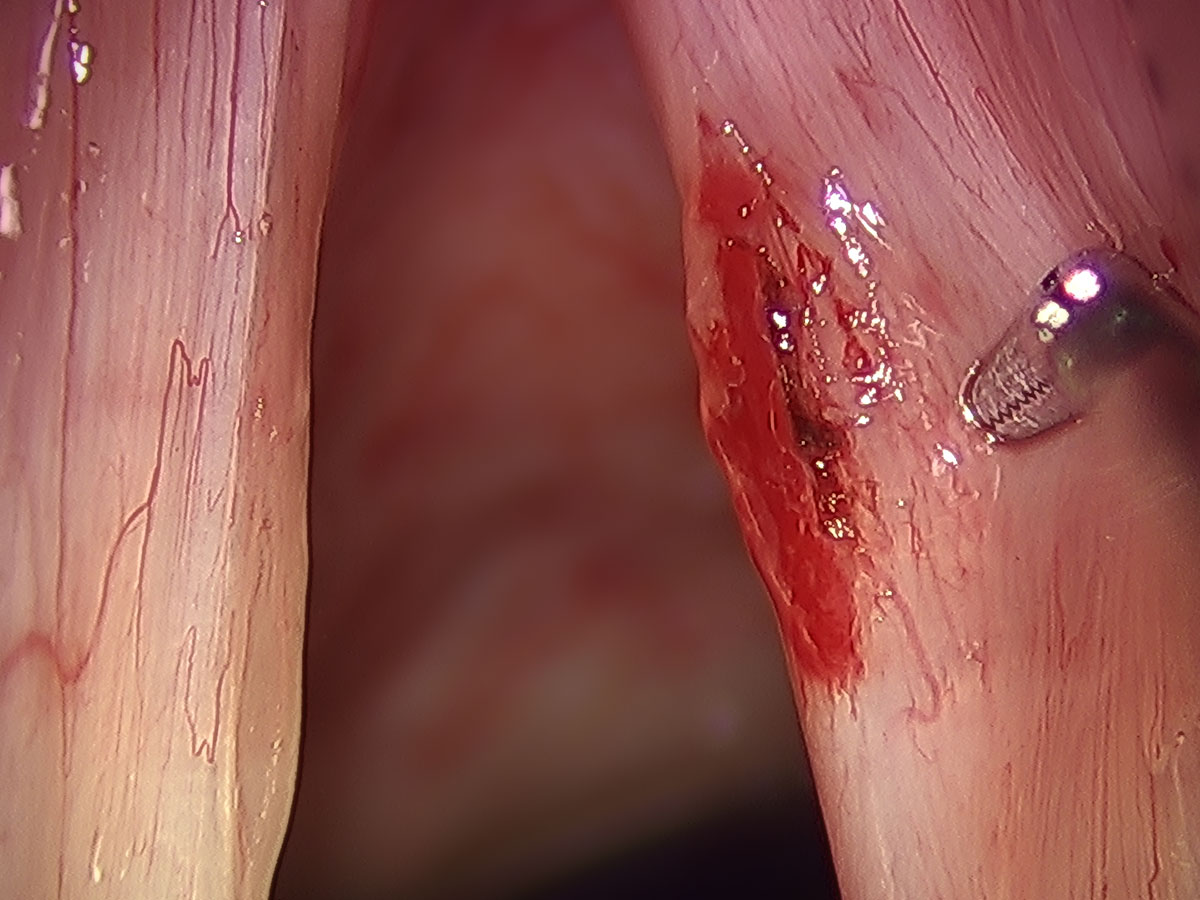
Whether the lesion is a cyst or a polyp, the surgical approach remains similar. It involves a general anaesthetic and microlaryngoscopy. There are reports of the use of serial office laser treatments to remove polyps or cysts but this should be strongly discouraged. Given the incredibly delicate and precise layered microstructure of the vocal folds and their unique function, all attempts should be made to preserve normal tissue. Such precision can only be obtained under microlaryngoscopy. With repetitive laser procedures there is the potential for injury to surrounding normal vocal cord tissue, which is not recoverable. This can lead to permanent hoarseness.
The surgery involves an epithelial cordotomy, which involves an incision of the lining of the vocal fold. Through this incision the cyst or polyp is carefully dissected and removed free. There is complete preservation of the underlying superficial lamina propria of the vocal fold. There is also maximal preservation of the overlying epithelium. With some patients there is reactive scarring on the opposite vocal fold. If that is the case, it may be necessary for that side to undergo a similar procedure to remove the abnormal tissue.
Following voice surgery there is a 1-2 week period of complete and absolute voice rest. This allows for full epithelial healing before voice therapy commences. Over the next six weeks the speech therapist will guide the increasing voice use and most patients are back at full voice use by six weeks following surgery.
When patients are assessed for this condition they are able to view similar lesions with both before and after results to get a feeling and comfort level for the type of surgery that is being recommended and the expected outcome.