The vocal folds have the most dense neurological wiring of any organ in the body outside the brain. It is possible for a patient to develop a deficit in the function of a nerve to the vocal cord. When this occurs the tremendous precision of the vocal folds is compromised with resultant hoarseness or extreme breathiness. In addition, patients can develop significant swallowing difficulties and choke on liquids. The most common causes of a unilateral vocal cord paralysis include surgery to the cervical spine, thyroid gland, parathyroid gland, lymph nodes in the neck or the carotid artery. Such an injury can also occur during surgery in the chest. Aside from these, other causes include lung cancer, skull base or neck tumours related to the nerve structure, trauma and then a group of patients where no cause is identified.
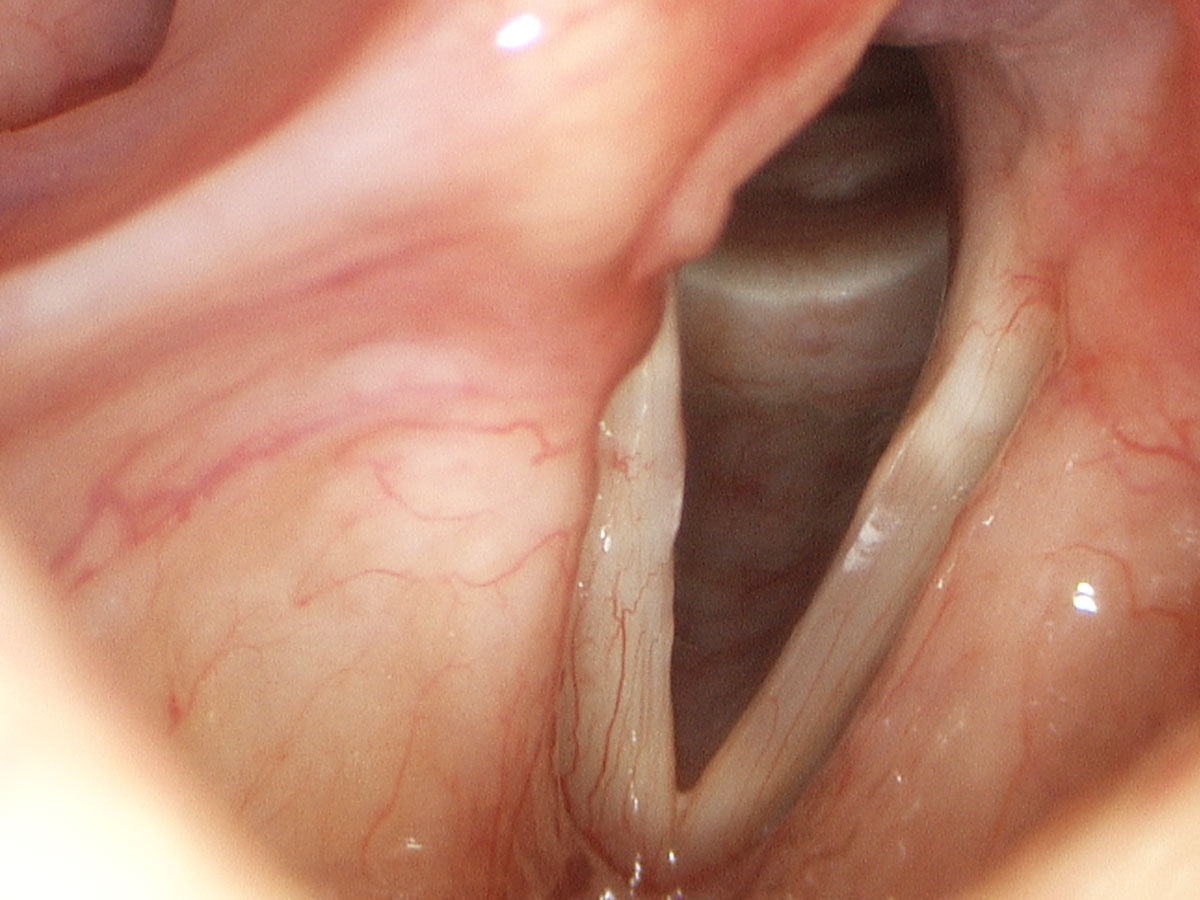
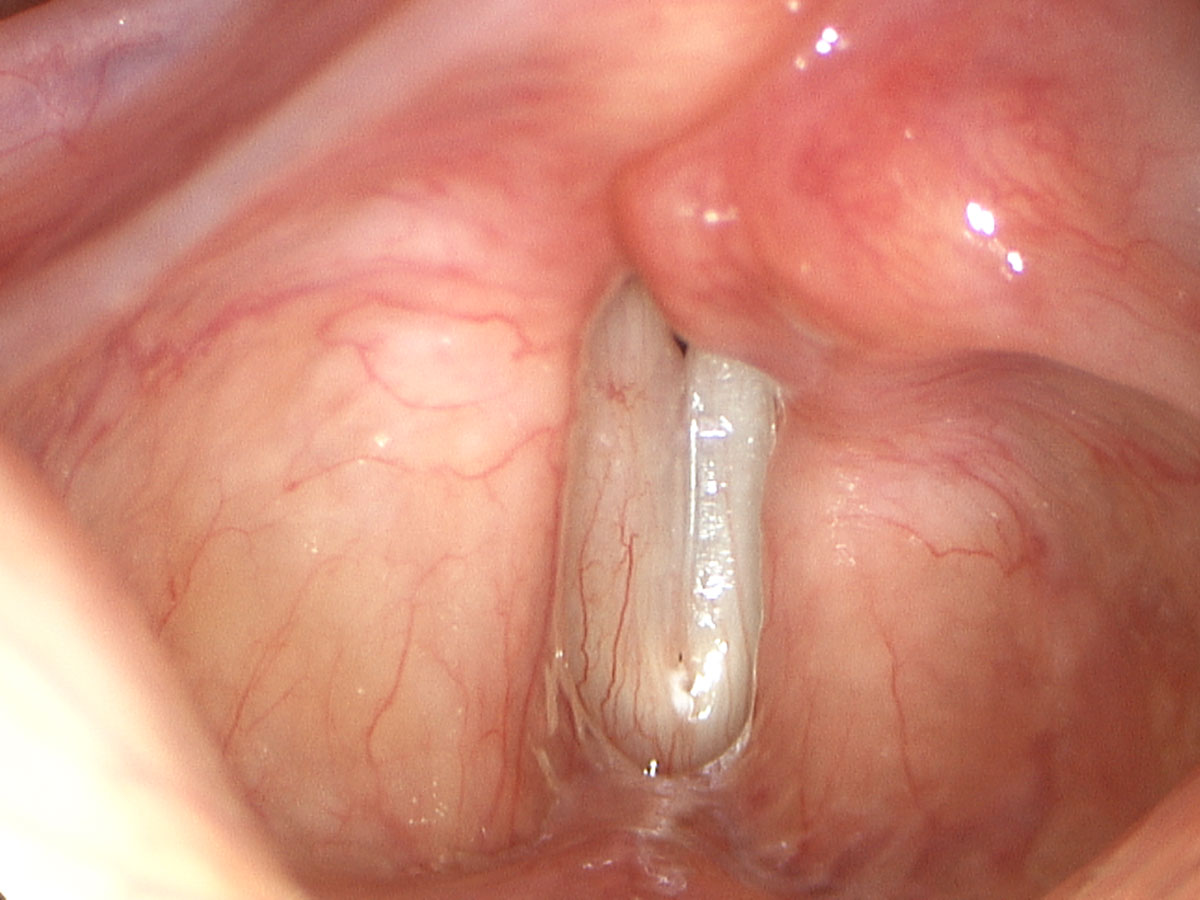
For such patients management is divided into two main areas. The first is the acute setting, which follows soon after the paralysis is realised. In this setting the innovative techniques employed by Dr Broadhurst allow for an immediate awake injection laryngoplasty. This involves anaesthetic in the mouth and throat followed by an injection of a hyaluronic acid gel into the paralysed vocal cord. The gel pushes the vocal cord into the midline where it would normally move for creating voice. Once held in the midline by the gel, the normal other side can close completely against the immobile vocal cord, allowing much more normal quality voice and airway protection. The gels available have varying degrees of duration of effect (residence time). Dr Broadhurst will decide which gel he feels is appropriate to provide a specified period of time for benefit from the injection.
One of the benefits of this gel that Dr Broadhurst utilises is its ability to be dissolved by an enzyme. An injection of an enzyme can dissolve the hyaluronic acid for an immediate removal of the product. This is sometimes used in the setting when a patient proceeds to a more formal, permanent reconstruction and any residual hyaluronic acid needs to be removed. The other setting that it can be used in is where an injection is placed in a suboptimal position. Fortunately, to date this has not occurred in Dr Broadhurst’s use of hyaluronic acid. In the unlikely event that it did occur, the enzyme can be injected into the suboptimally placed hyaluronic acid and it would then dissolve and be totally absent.
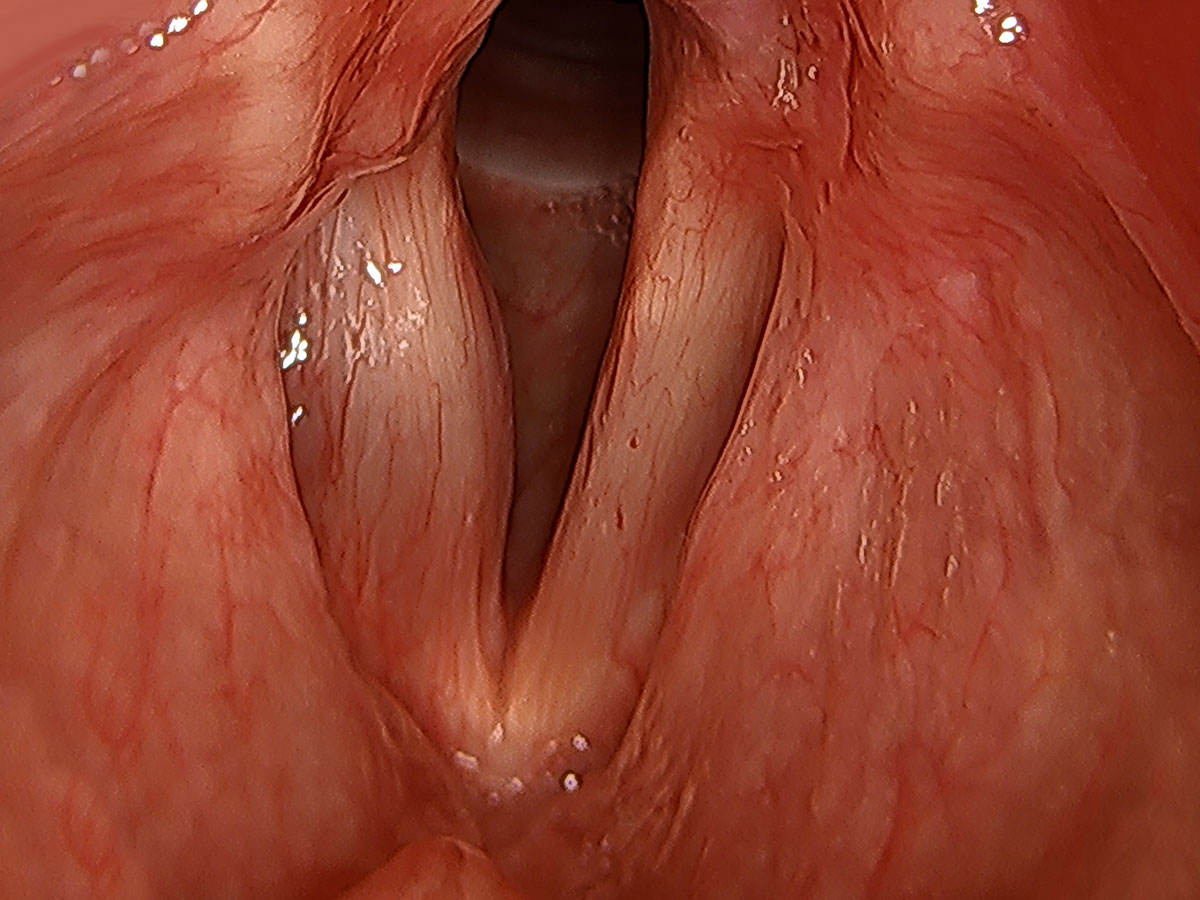
The second setting in managing patients with a paralysed vocal fold is in the long-term paralysis. This is the setting where there is no likelihood of nerve recovery. In that event careful office evaluation is undertaken to determine what the best long-term reconstructive option is. Long-term reconstruction options include moving the vocal cord into the midline with Gore-Tex or utilising this procedure in conjunction with movement of the arytenoid cartilage into the midline (adduction arytenopexy). An arytenoid adduction is another technique used to move the arytenoid cartilage into the midline. The reason Dr Broadhurst does not utilise the arytenoid adduction is that it tends to rotate the arytenoid toward the midline rather than move the whole cartilage into the midline. Moving the whole cartilage into the midline (adduction arytenopexy) provides a more anatomically normal position of the arytenoid for creating sound. Published research results show a clear benefit for patients undergoing an arytenoid procedure in the setting of paralysis over simply placement of an implant alone. There are pre-formed implants on the market (Montgomery implant). Using a pre-formed implant in the setting of a dynamic structure like the vocal fold is not an ideal situation in Dr Broadhurst’s opinion. By trying to apply a fixed shape implant to a vocal fold paralysis implies that all paralysed vocal folds are the same. This is certainly not the case and Dr Broadhurst prefers the precision of meticulously placed strips of Gore-Tex to achieve ideal medialisation over pre-formed implants.
Dr Broadhurst has the largest series of adduction arytenopexy procedures in permanent reconstruction of vocal cord paralysis outside of the USA where the procedure was developed. Dr Broadhurst often is invited to lecture on this topic, both nationally and internationally. While on staff at the Royal Brisbane Hospital he was fortunate enough to be able to introduce this technique into that hospital, which was a first in Australia.
Dr Broadhurst has an extensive collection of data on patients both before and after surgery for various types of vocal cord reconstruction. Keeping such data enables detailed analysis of patient outcomes and can provide new patients with estimates for their expected outcome.